Bilateral interstitial pneumonia and 2nd degree atrioventricular block as complications after COVID-19 infection
Main Article Content
Abstract
Objective: The epidemiological and clinical manifestations, pathogenesis, and complications in patients in the acute phase of coronavirus infection are described in detail. On the other hand, the term "prolonged COVID" was introduced in early 2020, representing a multisystemic disease that can occur even after a mild course of acute disease.
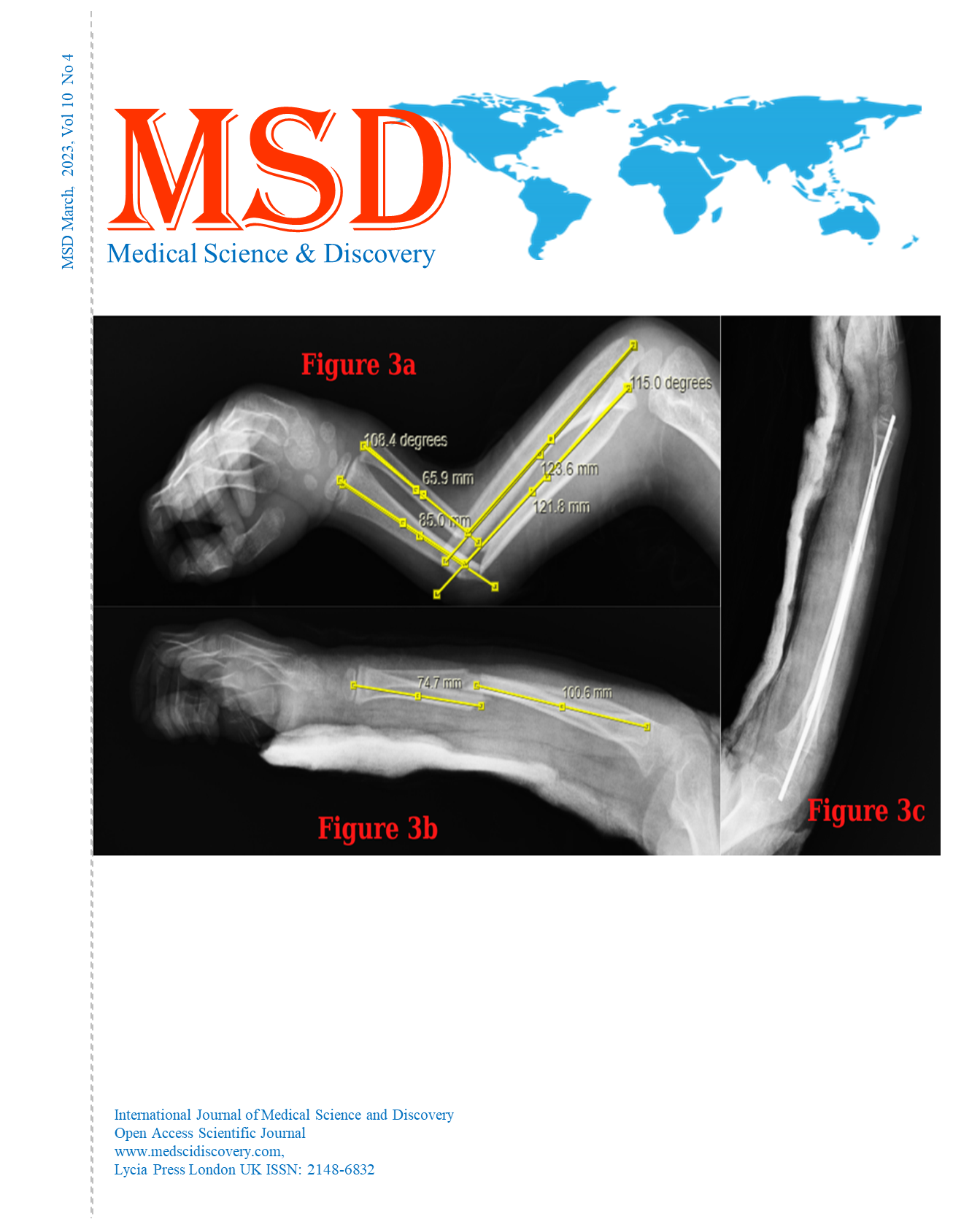
Case presentation: We present the case of a 61-year-old woman who reported severe dyspnea and was previously tested positive for coronavirus. The patient experienced worsening of the health condition again, and a chest X-ray showed changes that correspond to bilateral interstitial pneumonia, and high degree atrioventricular block (AV) was verified on an electrocardiographic record (ECG). After treatment with dual antibiotic therapy and implantation of a permanent electrostimulator (pacemaker), her condition significantly improved.
Conclusion: Approximately 10% of patients with COVID-19 may have symptoms persisting beyond three weeks, which presents as post-COVID syndrome. Primary healthcare professionals have a key role in the management of these patients. Research is needed to reveal the pathogenesis, clinical spectrum, and prognosis of post-COVID syndrome.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Accepted 2023-04-25
Published 2023-04-27
References
WHO. WHO Coronavirus disease (COVID-19) dashboard. See https://covid19.who.int/ (last checked 01.04.2023.)
Kingstone T, Taylor AK, O'Donnell CA, Atherton H, Blane DN, Chew – Graham CA. Finding the 'right' GP: a qualitative study of the experiences of people with long –COVID. BJGP open. 2020; 4(5).
Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): A review. JAMA. 2020; 324(8): 782–793. doi:10.1001/jama.2020.12839
Aiegbusi OL, Huges SE, Turner et al. Symptoms, complications and management of long COVID: A review. Journal of Royal Society of medicine. 2021; vol.114(9):428-442
Nikhra V. Living with “Long COVID 19”: The long – term complications and sequelae. Int J Clin Virol. 2021; 5: 011 -017.
NICE. COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19. NICE Guideline [NG188]. See https://www.nice.org.uk/guidance/ng188
Pavli A, Theodoridou M, Maltezou HC. Post – COVID syndrome: Incidence, clinical spectrum and chalanges for primary healthcare professionals. Archives of medical research 52. 2021; 575-581.
Fraser E. Long term respiratory complications of covid-19. BMJ. 3 Aug 2020, 370:m3001. doi:10.1136/bmj.m3001.
Zhao Y-M, Shang Y-M, Song W-B, et al. Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery. eClinicalMedicine - Lancet, 14 July 2020. doi: 10.1016/j.eclinm.2020.100463.
The prospective follow-up study of patients infected with the coronavirus, presented at the European Respiratory Society International Congress. 7 Sep 2020. Link – https://www.ersnet.org/the-society/news/covid-19-patients-suffer-long-term-lung-and-heart-damage-but-it-can-improve-with-time
Leulseged TW, Hassen IS, Edo MG, et al. Duration of supplemental oxygen requirement and predictors in severe COVID 19 patients in Ethiopia: A survival analysis. medRxiv preprint, 13 Oct 2020. doi: 10.1101/2020.10.08.2020912
Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (covid-19). JAMA Cardiol. 1 Nov 2020. 5:11, 1265-1273. doi: 10.1001/jamacardio.2020.3557.
Sardari A, Tabarsi P, Borhany H, et al. Myocarditis detected after COVID-19 recovery. Eur Heart J Cardiovasc Imaging, 1 Jan 2021, 22:1, 131-132. doi: 10.1093/ehjci/jeaa166.
Babapoor-Farrokhran S, Batnyam U, Wiener PC, et al. Atrioventricular and sinus node dysfunction in stable COVID-19 patients. SN Compr Clin Med. 2020 [Epub ahead of print]: 1–4. doi: 10.1007/s42399-020-00497-5
Al-Assaf O, Mirza M, Musa A. Atypical presentation of COVID-19 as subclinical myocarditis with persistent high-degree atrioventricular block treated with pacemaker implant. HeartRhythm Case Rep. 2020; 6(11): 884–887. doi: 10.1016/j.hrcr.2020.09.003.
Wojewoda K, Tarkowski A, Wysokinska K et al. Syncope due to third – degree atrioventricular block as the only manifestation of miocarditis following COVID – 19 infection. Polish heart journal. 22 Sept 2021.
Varatharaj A, Thomas N, Ellul MA, et al., CoroNerve Study Group. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry, Oct 2020, 7:10, 875-882. doi: 10.1016/S2215- 0366(20)30287-X.
del Rio C, Collins LF, Malani P. Long-term health consequences of COVID-19. JAMA. 5 Oct 2020. doi: 10.1001/jama.2020.19719.
Meppiel E, Peiffer-Smadja N, Maury A, et al. Neurologic manifestations associated with COVID-19: a multicentre registry. Clin Microbiology and Infection, November 12, 2020. doi: 10.1016/j.cmi.2020.11.005.
Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endothelitis in COVID-19. Lancet, 2 May 2020, 95:10234, 1417-1418. doi: 10.1016/S0140-6736(20)30937-5.